Abstract
INTRODUCTION Patients with hematologic malignancies (HM) experience high physical and psychological symptom burden. However, they rarely access Palliative Care (PC) services. Some authors affirm that patients with HM receive an aggressive end-of-life (EoL) care. Our objective was to describe the quality of EoL care in hospitalized patients with HM who died in our center in 2018-2019. We compared the EoL management between patients with a Hematology exclusive follow-up and those who had a PC complementary approach. We searched for variables associated with a score for aggressiveness of end-of-life care (SAELC).
PATIENTS AND METHODS
This is a unicentric, observational, retrospective study. We included all inpatients with HM who died between 01/01/2018 and 31/12/2019 (N = 100). We reviewed medical records to collect baseline demographics, HM features, diagnostic tests, and transfusion requirements in the last weeks of life, and EoL care indicators: PC follow-up, cancer therapy use, emergency room (ER) visits, hospital, and intensive care unit (ICU) admissions and days in hospital in the last month of life. Prescribed drugs on the date of death were also collected. Data were summarized using descriptive statistics. Parametric and non-parametric tests were used as appropriate in the inferential analysis.
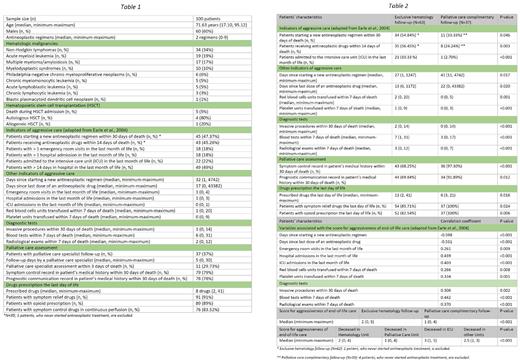
RESULTS The median age was 71.63 years and 60% were males (table 1). The most frequent HM were non-Hodgkin lymphomas (34%).
In the last month of life, 47.4% started a new antineoplastic regimen, 18% had more than 1 ER visit, 18% had more than 1 hospital admission and 22% were admitted to the ICU; 45.3% received antineoplastic drugs within 14 days of death and 49% spent more than 14 days in hospital in their last month. These indicators form a SAELC (0 = best, 6 = worst).
Invasive procedures within 30 days of death (median = 1), blood tests (median = 6) and radiological exams (median = 2) within 7 days of death were frequent.
Regarding PC follow-up, 37 patients accessed PC services and 11 had a PC assessment within 3 days of death. In the last day of life, the median prescribed drugs was 8, 91% had symptom-relief drugs, and 89% had opioid prescription; 49% died in the Hematology Unit, 28% in the PC Unit, 21% in the ICU and 2% in other medical Units.
When they were followed by PC, fewer patients started a new antineoplastic regimen within 30 days of death (32.35% vs. 54.84%, p = 0.046), received antineoplastic drugs within 14 days of death (24.24% vs. 56.45%, p = 0.003) and were admitted to the ICU in the last month of life (2.70% vs. 33.33%, p < 0.001) (table 2).
Other indicators of aggressive care (days since starting a new antineoplastic regimen, days since last dose of an antineoplastic drug and transfusion requirements) and number of diagnostic tests were more favorable when patients were assessed by PC. A higher proportion of symptom control and prognostic communication record, as well as simplified drug prescription were observed when patients had a PC approach.
The number of days since starting a new antineoplastic regimen and days since last dose of an antineoplastic drug had an inverse correlation with the SAELC. Direct correlations were observed between the SAELC and ER visits, hospital, and ICU admissions in the last month of life, transfusion requirements within 7 days of death and number of diagnostic tests. The median SAELC was lower when patients had a PC follow-up (1 vs. 2, p < 0.001).
DISCUSSION AND CONCLUSIONS
We found our patients had several ER visits, hospital, and ICU admissions, and received cancer treatments in the last weeks of life. We identified a lack of PC involvement, with short follow-ups and late assessments.
Our study showed an improvement in many indicators of aggressive care when there was a PC follow-up.
A more favorable symptom control, prognostic communication, and drug prescription the last day of life were observed when PC was involved.
Less chemotherapy use and accessing PC services were associated with a lower SAELC.
The main limitations are including only inpatients and the retrospective unicentric design. A prospective study incorporating outpatients would provide a comprehensive view of the EoL care of our patients.
Regarding the special features of patients with HM, specific indicators of aggressive care should be established to design a tailored SAELC for them.
The hematology community need to develop programs to improve the quality of EoL care for patients with HM.
Disclosures
Alonso Dominguez:Incyte: Research Funding; Pfizer: Research Funding; Astellas: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal